Every summer a microscopic predator resurfaces in the headlines, blamed for a handful of devastating deaths yet lurking in warm ponds, rivers, taps, and even backyard hoses worldwide. Naegleria fowleri—the so-called brain-eating amoeba—is vanishingly rare, but when it reaches the human brain it kills more than 97 percent of its victims. This report explains how the organism lives, how it overcomes the immune system, why cases are rising northward with climate change, and—most critically—how communities and individuals can block its path.
Ecology and Life Cycle of Naegleria fowleri
Thermophilic habitat
N. fowleri is a free-living amoeboflagellate that thrives between 25 °C and 46 °C, surviving brief spikes to 50+ °C by encysting. It colonises warm freshwater lakes, rivers, geothermal pools, poorly chlorinated swimming pools, pipes, hoses and distribution mains where residual chlorine is low. Surveys in Arizona wells found the amoeba in 8% of source samples, while Australian investigators recently detected it in municipal tap water after a heatwave.
Morphological stages
The amoeba alternates among three forms: the feeding trophozoite, a transient biflagellate, and a resilient cyst. Trophozoites divide every 2–3 h, switch to flagellates when nutrients drop, and encyst when temperatures fall or disinfectant rises.
Life cycle of Naegleria fowleri showing environmental stages, infection through the nasal mucosa, and progression to brain infection causing primary amebic meningoencephalitis
Image 88: CDC life-cycle schematic illustrating trophozoite, cyst and flagellate stages and nasal entry route.
Pathogenesis: From Nasal Splash to Fulminant PAM
Chemotaxis and invasion
While millions of humans inhale freshwater daily without incident, N. fowleri follows acetylcholine gradients released by olfactory neurons, acting through a surface GPCR homologous to human mAChR1. Within hours the amoeba climbs the olfactory nerve, crosses the cribriform plate, and reaches the olfactory bulbs, bypassing the blood–brain barrier.
Immune evasion
Highly pathogenic strains display CD59-like proteins that block membrane-attack-complex assembly, shed complement on extracellular vesicles, and resist cytokine lysis. Neutrophils respond with oxidative bursts and extracellular traps, but unopsonised trophozoites frequently escape. Once in the brain, Nfa1 and actin-rich food-cups (amoebastomes) trogocytose live neurons, causing hemorrhagic necrosis and fatal intracranial hypertension within 7–10 days.
Microscopic image of Naegleria fowleri trophozoites showing their characteristic amoeboid shape and internal structures
Image 85: Light-microscopy view of violet-stained N. fowleri trophozoites showing vacuolated cytoplasm and central karyosome.
Clinical course
Primary amoebic meningoencephalitis (PAM) incubates 1–9 days, beginning with fever, headache and nausea, then rapidly progressing to stiff neck, seizures, hallucinations and coma; median time to death is five days. Histology reveals acute necrotising meningoencephalitis with trophozoites amid hemorrhage and granulocytes.
Global Epidemiology and Climate Trends
Since 1962 the United States has confirmed 167 cases, with only four survivors. Worldwide literature review tallied 381 cases through 2018, increasing 1.6% annually and expanding into higher latitudes. In 2024–25 clusters in Kerala, Pakistan, Israel, Missouri and Queensland underscore climate-driven geographic spread as surface waters warm and drought lowers lake levels.
Demographics and exposure settings
- 76% of patients are male, median age 14; children’s porous cribriform plates may ease invasion.
- 58% linked to lake/pond swimming, 10% to water sports, 9% to nasal irrigation with tap water, and 12% to inadequately chlorinated pools.
- Household plumbing outbreaks in Louisiana (2011) and Arizona (2013) arose from warm chloramine systems with residuals <0.1 mg/L.
Diagnostics and Therapeutics
Rapid diagnosis
Early CSF wet-mount may reveal motile trophozoites; PCR targeting ITS or 5.8S rDNA is now the gold standard and can detect <1 organism in CSF within hours. Novel RT-qPCR assays detecting amoebic small RNA biomarkers promise even earlier blood-based diagnosis.pmc.ncbi.nlm.nih+1
Treatment protocols
Survival hinges on swift, multi-drug regimens: intravenous and intrathecal amphotericin B, azithromycin, rifampin, fluconazole/posaconazole, miltefosine, dexamethasone, hypothermia (32–34 °C), and aggressive intracranial pressure control. Since CDC released investigational miltefosine in 2013, all U.S. survivors have received it within 48 h.
Drug research
In vitro screens show miltefosine, chlorpromazine and voriconazole outperform amphotericin B in trophozoite kill; experimental mice reached 55–75% survival with combination therapy. Actin and Nfa1 knock-down studies suggest future RNA-targeted approaches.
Prevention and Public Health Measures
Water-system controls
Maintaining free chlorine ≥1 mg/L at 25 °C achieves ≥2-log cyst inactivation (CT ≥ 25 mg·min/L); UV doses ≥63 mJ/cm² likewise ablate cysts. Utility “chlorine conversions” in Louisiana eliminated N. fowleri from distribution mains after 60 days of boosted chlorine and unidirectional flushing. WHO guidance urges <25 °C distribution temperatures and residual disinfectant at all taps.
Recreational guidance
- Avoid jumping, diving or submerging the head in untreated warm freshwater; wear nose clips or keep head above water
- Rinse nasal devices only with sterile, distilled, or boiled-then-cooled water; household filters must be ≤1 µm absolute
- Backwash and chlorinate pools to ≥1 ppm free chlorine; maintain spas at ≥3 ppm with ≥30 °C avoided.
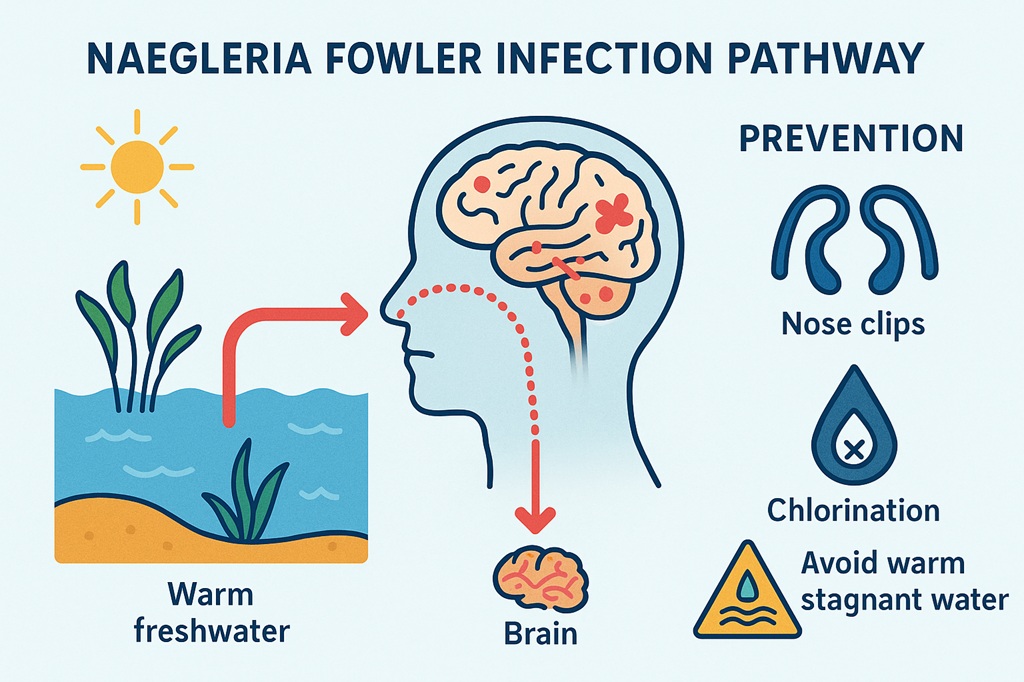
Infographic: How Naegleria fowleri infects and how to prevent it
Image 89: Generated infographic summarising infection pathway and personal prevention strategies (nose clips, treated water, avoiding warm stagnant sources).
Conclusion
N. fowleri infections remain rare—drowning, for instance, is a thousand-fold likelier fatal hazard during a lake outing—but climate warming, aging water infrastructure, and recreational patterns are aligning to push the amoeba into new regions. Because effective chemotherapeutics exist only when administered early, the public-health priority is two-fold: engineer water systems and recreational venues that deny the amoeba warm, low-chlorine refuges, and train clinicians to recognise PAM hours, not days, after symptom onset. Adhering to disinfectant residuals, cooling or shading storage, flushing dead-ends, and practicing simple nasal precautions can block every step of the amoeba’s journey from puddle to brain. Rapid diagnostics, strategic drug stockpiles, and climate-adaptive surveillance will determine whether the next generation reads about N. fowleri primarily in textbooks—or in obituaries.